The Mini-Gastric Bypass or single anastomosis gastric bypass, is an effective and well-established procedure which combines some of the properties of a gastric sleeve and a standard gastric bypass. The upper part of the stomach is divided into a tube, similar to the top three quarters of a sleeve, and then joined to a loop of intestine.
The mini-gastric bypass can be used as a primary weight loss procedure. It can also be used in patients who have had previous gastric banding or sleeve surgery but have been unsuccessful with weight loss, or who have had band-related complications and have decided on revision surgery.
It is not ideally suited to patients with symptoms of reflux disease (severe heartburn that needs medication).
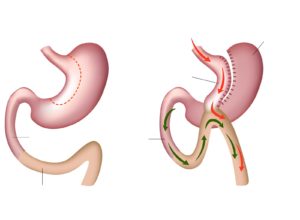 In this operation the top of the stomach is stapled to form a thin tube (30ml to 50ml in size). The thin tube becomes the new, smaller stomach and is completely separate to the rest of the stomach. This stomach is then sewn to a loop of the small intestine, bypassing the first part of the intestine called the duodenum and approximately 150–200cm of the bowel. The rest of the stomach and upper part of the small intestine remains in the body but is no longer used for food digestion.
In this operation the top of the stomach is stapled to form a thin tube (30ml to 50ml in size). The thin tube becomes the new, smaller stomach and is completely separate to the rest of the stomach. This stomach is then sewn to a loop of the small intestine, bypassing the first part of the intestine called the duodenum and approximately 150–200cm of the bowel. The rest of the stomach and upper part of the small intestine remains in the body but is no longer used for food digestion.
The mini bypass procedure helps you to lose weight in different ways:
- By reducing the feeling of hunger through altered gut to brain signalling
- By enabling an earlier feeling of satiety and fullness when eating a meal resulting in a healthy portion size
- By decreasing the amount of calories you absorb from your food as a result of bypassing 150 to 200cm of the upper part of the small intestine
Rerouting of the food stream produces changes in gut hormones that reverse one of the primary mechanisms by which obesity-induced type 2 diabetes occurs.
Long-term effects of the Mini-Gastric Bypass
Several studies have been carried out and published on the long term (over 5 years) effects of mini-gastric bypass surgery. Two years after the surgery, weight loss is 75-85% of excess body weight; five years after the surgery, the excess body weight loss is 70-75%.
Weight loss with mini-gastric bypass is as good, if not better, than that achieved with standard gastric bypass surgery in people with a higher BMI.
Many diseases connected to being overweight like sleep apnoea, type 2 diabetes, joint diseases, high blood pressure or polycystic ovary syndrome (PCOS) improve or disappear as a result of the surgery.
Important! Long term effects of any gastric surgery are reliant on a patient making the necessary changes to lifestyle, particularly in relation to diet and exercise.
Complications after Mini-Gastric Bypass surgery
As with any surgical procedure, the mini-gastric bypass operation has a risk profile which is important to understand before proceeding. The following is a comprehensive list of issues which can occur. Most of these complications are very rare and 90–95% of patients have no issues. This list is extensive and is not intended to worry you, but simply inform you about the range of possible complications, regardless of how rare the issue may be.
Possible early complications:
Serious complications are those requiring emergency reoperation or any other intervention like endoscopy, transfusion of blood or blood components or mandating stay in the hospital for more than 7 days.
In our practice the most likely earlly complication has been postoperative bleeding (1% of patients). Usually the bleeding stops itself and isn’t so great that the blood transfusion is needed.
Other early complications (occurrence 0,5%) may be: peritonitis; thrombus of deep veins and lung artery; myocardial infarction; pneumonia; abdominal abscess; wound infections; hernias at the surgical site, ulcers.
90% of complications that need additional special medical care, occur within 48 hours after surgery, when patient is still in hospital.
Late complications & side effects after mini gastric bypass
Internal hernia – Risk of internal hernia is considerably lower after mini-bypass (1:500) than after standard gastric bypass (2:100). Occasionally the loops of bowel in the abdomen can become entangled and get stuck. If this occurs, a reoperation is required to fix the problem.
Adhesions – Any procedure in the abdomen can cause adhesions (scar tissue). This can occur any time after the operation and can sometimes cause problems with the bowel getting stuck or twisted. This may require hospitalisation and may even require re-operation.
Gastro-esophageal reflux – If reflux occurs post-operatively some patients may require acid-suppressing medication. This operation should be avoided for those people with severe symptoms of reflux prior to surgery.
Dumping syndrome – Dumping syndrome is a group of signs and symptoms that usually occurs due to poor food choices. It is the result of high sugar foods passing too quickly into the small intestine. Symptoms can include cramping, nausea, dizziness, weakness and fatigue. Dietary advice to avoid dumping is provided by the clinic’s dietician.
Malabsorption of vitamins and minerals – Low levels of iron, B12 vitamin and other micronutrients can occur even if recommendations for supplementation are followed. For this reason, regular follow-up visits and blood tests once a year are strongly recommended. Risk of malnutrition.
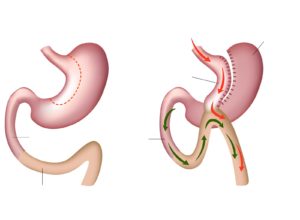 In this operation the top of the stomach is stapled to form a thin tube (30ml to 50ml in size). The thin tube becomes the new, smaller stomach and is completely separate to the rest of the stomach. This stomach is then sewn to a loop of the small intestine, bypassing the first part of the intestine called the duodenum and approximately 150–200cm of the bowel. The rest of the stomach and upper part of the small intestine remains in the body but is no longer used for food digestion.
In this operation the top of the stomach is stapled to form a thin tube (30ml to 50ml in size). The thin tube becomes the new, smaller stomach and is completely separate to the rest of the stomach. This stomach is then sewn to a loop of the small intestine, bypassing the first part of the intestine called the duodenum and approximately 150–200cm of the bowel. The rest of the stomach and upper part of the small intestine remains in the body but is no longer used for food digestion.